The health sector had years to improve training of locals. Now they call for immigration. But that is not a solution. The only long-term answer is more training and better retention of existing staff
- Reliance on overseas-trained medical staff has allowed the NHS to get away with a long-term failure to plan for the training of the medical staff we need.
- The NHS is struggling to retain UK doctors in part due to a combination of low morale and high workloads that has, in recent years, been made more acute by rapid population growth, itself driven by very high levels of immigration (net non-UK immigration averaged just over 300,000 per year- 2010-20).
- As a result of these and other factors, the UK’s health service is more reliant on overseas doctors and nurses than most comparable healthcare systems in the developed world.
- The health sector’s standard response is to call for immigration. But it is immoral to be taking medical professionals from countries where medical needs are far greater than the UK’s.
A failure to train UK workers
The British Medical Journal now says hundreds of NHS posts remain unfilled. If so this is mainly due to a failure by the health sector itself, after years of warnings, to train the many UK applicants who would like these jobs. Addressing this should be the priority.
As consultant surgeon J. Meirion Thomas has said, ‘tens of thousands of British students with the required A-level grades are rejected only because of insufficient training slots’.
Meanwhile, UCAS figures showed that nearly 2 in 3 UK applicants for nursing courses were turned down (2010-19) while tens of thousands of nurses were brought in from abroad on the basis of “shortage'”. This is madness.
The independent Migration Advisory Committee (MAC) has also criticised the government and health sector specifically for failing to maintain the supply of UK-trained nurses. Britain is also not training enough doctors.
– In 2013, the MAC noted ‘the absence of a specific training pathway to produce middle-grade doctors’ in the UK (see p.90 of report).
– Until 2014, over 30,000 UK applicants for nursing courses were turned away annually, according to the Nursing Labour Market Review.
– Former MAC Chair Sir David Metcalfe said in March 2016: “There is no good reason why the supply of nurses cannot be sourced domestically. There seems to be an automatic presumption that non-EEA skilled migration provides the health and care sector with a ‘Get out of Jail Free’ card.”
– The MAC said in July 2016: “[We have] consistently emphasised the need to raise British human capital and thereby lessen employer dependence on immigration. The IT, engineering and health sectors invest insufficiently in UK residents.”
Meanwhile, the current shortage of nurses in England is closely linked to the decision by the government to cut training places.
Medical industry groups say there is a need to stop relying on immigration to fill skills needs in the NHS and train up UK recruits.
– As the Royal College of Physicians has noted: “The long-term focus needs to be developing the homegrown healthcare workforce.”
– The British Medical Association said in 2013: ‘The principle of reducing reliance on migrant workers and training and up-skilling UK resident workers to fill workforce gaps is entirely valid.’
Retention of UK doctors
It is also true that applications to UK medical courses have fallen recently, that more than half of junior doctors finishing basic training last year did not continue on an NHS career path and that the number of UK doctors leaving to work in places such as Australia and New Zealand appears to be rising.
There may be a number of reasons for this, including worsening morale, and rising workloads. The latter factor is clearly exacerbated by what the BMA call a ‘growing demand for health services’. ‘The population is getting bigger and older, and expectations are rising along with the costs of meeting them’, noted the Institute for Fiscal Studies recently.
Of course, a key reason behind the current rapid rate of population growth is net migration of nearly quarter of a million a year. As a rough indication of this, there were nearly 750,000 new migrant GP registrations in England, Northern Ireland and Wales in 2015/16 – the highest on record (ONS statistics). Cutting immigration to a sustainable level is an obvious way by which to reduce the rising demand on the NHS.
Additionally, as the MAC has noted, the government must redouble its efforts to provide ‘sufficient incentive and opportunity’ to retain more staff in the NHS in future.
The NHS has a relatively high reliance on foreign-trained staff. Data released in 2019, which revealed that 35% of doctors licenced to practice in the UK had obtained their qualifications overseas (see doctors’ letter to South African Medical Journal).
– A report by NHS Providers has found that the NHS imports significantly more doctors and nurses than Germany, France, Spain, Canada, the US, Sweden and the Netherlands.
– Only Ireland, Israel, Norway, New Zealand and Australia are more reliant on foreign-trained staff than the UK.
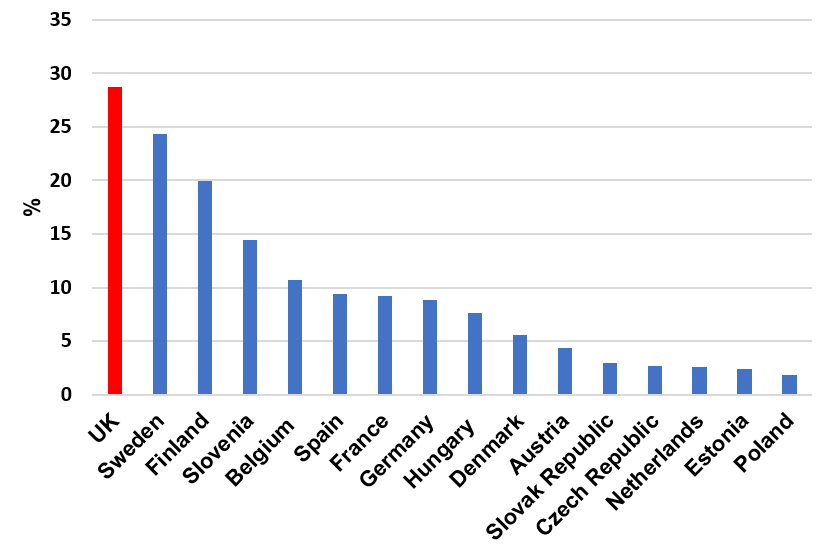
– In the Netherlands (which has one of the top five healthcare systems in the world) the percentage of doctors who were foreign-trained in 2013 was 2.6% in 2013, compared to 28.7% for England. (Health Foundation report– see figure R, p. 15).
Percentage of doctors who were foreign-trained, 2013.
It is immoral to take healthcare staff from countries that need them more than the UK
How can we justify taking healthcare staff from countries that may need them far more than we do?
- A letter written recently by two doctors and published in the South African Medical Journal blamed the UK’s visa and immigration policy for the poaching of health workers from the world’s poorest countries. Professor Johannes Fagan from the University of Cape Town and Professor Mahmood Bhutta from the Royal Sussex County Hospital described the poaching of medical professionals from the world’s poorest regions as ‘insensitive’ and ‘morally questionable’.
- An article in the British Medical Journal published in January 2021 argued that large-scale migration [of physicians] has numerous consequences which include increased mortality associated with inadequate physician supply in low and middle-income countries.
- An international conference in Kampala in 2008 that called on richer countries to ‘give high priority and adequate funding to train and recruit sufficient health personnel from within their own country’ (Kampala Declaration).
- In Dublin in 2017, the Global Forum on Human Resources for Health emphasised the need for developing countries to retain their own healthcare workforces (Dublin Declaration).
The only longer-term solution, which would also have the benefit of easing concerns about language difficulties, is to restore strict and reasonable limits on the number of work permits issued to the health sector and address our continued failure to provide opportunities to our own young people to work in it.
